For the past few months, I have been working on an article about dietary management and patienthood in twentieth-century diabetes care. One key theme that has reoccurred throughout this research might be summed up by the question: “balance at what cost?” This is a question that patients and practitioners have had to ask consistently (if implicitly) since the 1920s, and I believe its history may have something to contribute to present discussions.
Balance: A Bit of Everything or Denial of Some Things?
Whether in popular culture or medical discourse, achieving and maintaining balance has frequently been discussed in overwhelmingly positive terms.
For patients with diabetes, medical advice for much of the twentieth and twenty-first centuries has been that metabolic balance is potentially life-saving.[i] That is, glycaemic control has been seen as the best safeguard against a range of short-term problems, as well as the means to prevent the onset of – or reduce the likelihood of developing – devastating long-term complications.
Yet, whilst we might associate balance with phrases like “all things in moderation”, balance in diabetes care has historically been construed in terms of restriction and regulation. Dietary management, that is, has often entailed either removing, carefully controlling, or substantially increasing the intake of certain foodstuffs. Amongst other things, hyper-vigilance and the inability to have a little of everything have been two of the costs associated with balance for individuals (and often their familial and social relations).
Changing Dietary Regulations
This is not to say that patterns of dietary prescription have remained static over time, especially for patients who required insulin. (Weight reduction through calorie control remained a constant imperative for overweight patients not using insulin.)
For instance, in the first few decades of the twentieth century, doctors discussed metabolic balance in relation to a careful restriction of carbohydrates. In fact, in some cases this even extended to banning certain foodstuffs. Lists of “forbidden foods” were often included on dietary sheets, and one doctor even declared that he had a “feeling that it is better for the patient to forget about the taste of bread altogether than be exposed to the temptation when he takes a fraction.”[ii]
These strictures altered considerably in following decades. During the 1930s and 1940s, doctors began to prescribe higher carbohydrate allowances, and in the following decades they dropped careful fat and protein regulation to help reflect more “normal” dietary patterns. After two decades worth of debate about the role of “free diets” in care, higher fibre intakes became a feature of discussions in the 1970s and 1980s, following the testing of theories designed in colonial sites of research. By century’s end, programmes for “normalisation” slowly began to move to the fore, resulting in strategies like DAFNE.[iii] Gradually, “forbidden” foods became controlled foods.
Calculating Costs
Regardless of these moving goal posts, patients and their families rarely adhered fully with their medical instructions. For some, this was simply a case of not being able to afford diets. The financial cost of diabetes diets regularly ran considerably higher than average expenditure on non-medical diets.
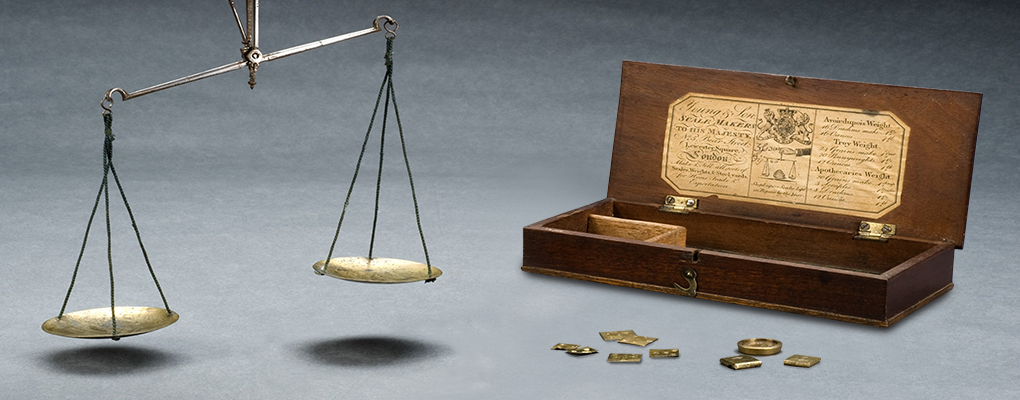
For other patients, the logistics of careful management were just as much of a barrier. Surveillance – with its constant vigilance, measurement, inscription and assessment – required more than considerable energy. It also demanded action, and access to a whole material culture. (Pens, records, dietary sheets, scales, jugs, and urine testing equipment.) The time and materials required were rarely accessible in the workplace, and regulating an individual’s diet often had unacceptable consequences for spouses, families, employers, and friends. Indeed, for patients regulating their diet in public, one result might be to mark them out, risking negative comments, social awkwardness and anxieties, as well as problems at social events, such as meals or celebrations. Under such circumstances, patients were either physically unable to manage their diets, pressured into certain actions, or encouraged to weigh their priorities and find (quite rationally) that other relationships and activities were worth the possible costs.
This also to say nothing about the extent to which prescriptions were adapted for cultural, class-based, or dietary preferences. Or, indeed, to discuss palatability. As one patient (who was also a doctor) challenged readers in The Lancet: “you try getting through 3-4oz butter with 1oz of bread to spread it on!”[iv]
Patients and Costing Balance
What I have taken away from this research is that many of the costs that follow the pursuit of balance are deeply embedded into social and cultural life, and can’t all be altered by educational, motivational, or bureaucratic programmes and imperatives.[v] The challenges of the past, in other words, are not dead, but are in many respects still with us.
In fact, we might ask whether there is a broader discussion to be had, one concerning the values attached to balance, and the extent to which reasons for patients not following advice should be conceived as “problems”. In many respects, this has been the starting point for many strategies designed to investigate and improve “compliance” and “adherence” in the past four decades.[vi]
To be sure, I believe that patient education is vital. Equally, co-operation between health care teams, patients and families is often integral to effective care, just as glycaemic control can be protective of long-term health. (Though not a guarantee.)
Nonetheless, at some point it will be necessary to consider the limits to these strategies, and – to a certain degree – the desirability of consistent attempts to problematize and alter behaviour. For those of us without the condition, it is also worth thinking clearly about the costs involved in management before rushing to moral judgement. One patient (again a practitioner) perhaps put it best when writing just after the Second World War:
“Each meal should be an elegant satisfaction of appetite rather than a problem in arithmetic and a trial of self-abnegation”.[vii]
Things have changed significantly since 1946, but daily challenges to patients are still considerable, and the mental, emotional and physical affects of management remain.
Notes
[i] Diabetes UK, ‘Self-Monitoring of Blood Glucose Levels For Adults With Type 2 Diabetes’, Diabetes UK Online, 2016. Available at: https://www.diabetes.org.uk/About_us/What-we-say/Diagnosis-ongoing-management-monitoring/Self-monitoring-of-blood-glucose-levels-for-adults-with-Type-2-diabetes/. Accessed on: 25th March 2016.
[ii] George Graham, ‘On the Present Position of Insulin Therapy’, The Lancet, Vol.204, 1924, 1265-6.
[iii] Or Dose Adjusted For Normal Eating: Anon, ‘DAFNE’, DAFNE Online, 2016. Available at: http://www.dafne.uk.com. Accessed on 25th March 2016.
[iv] Anon, ‘Disabilities: 21. Diabetes’, The Lancet, Vol. 253, 1949, p.116.
[v] Which have been popular solutions of the recent past: NHS England, Action on Diabetes, (January 2014). Online Document. Accessed on 16 June 2015. Available at: https://www.england.nhs.uk/ourwork/qual-clin-lead/diabetes-prevention/action-for-diabetes/. With some notable successes: R.P. Narayanan, J.M. Mason, J. Taylor, A.F. Long, T. Gambling, J.P. New, J.M. Gibson, R.J. Young, ‘Telemedicine to improve glycaemic control: 3-year results from the Pro-Active Call Centre Treatment Support (PACCTS) trial’, Diabetic Medicine, 2012. Available online: http://0-onlinelibrary.wiley.com.lib.exeter.ac.uk/enhanced/doi/10.1111/j.1464-5491.2011.03352.x.
[vi] Jeremy A. Greene, ‘Therapeutic Infidelities: ‘Noncompliance’ Enters the Medical Literature, 1955-1975’, Social History of Medicine, Vol.17, 2004, 327-43.
[vii] C.C. Forsyth, T.W.G. Kinnear, and D.M. Dunlop, ‘Diet in Diabetes’, BMJ, Vol.1, 1951, p.1099.